Ulcerative Colitis Diet: What foods to eat? What to avoid?
(For private circulation only. For the use of patients at Life Force. Copyright © 2004 -2009, Dr. Rajesh Shah. All rights reserved.)
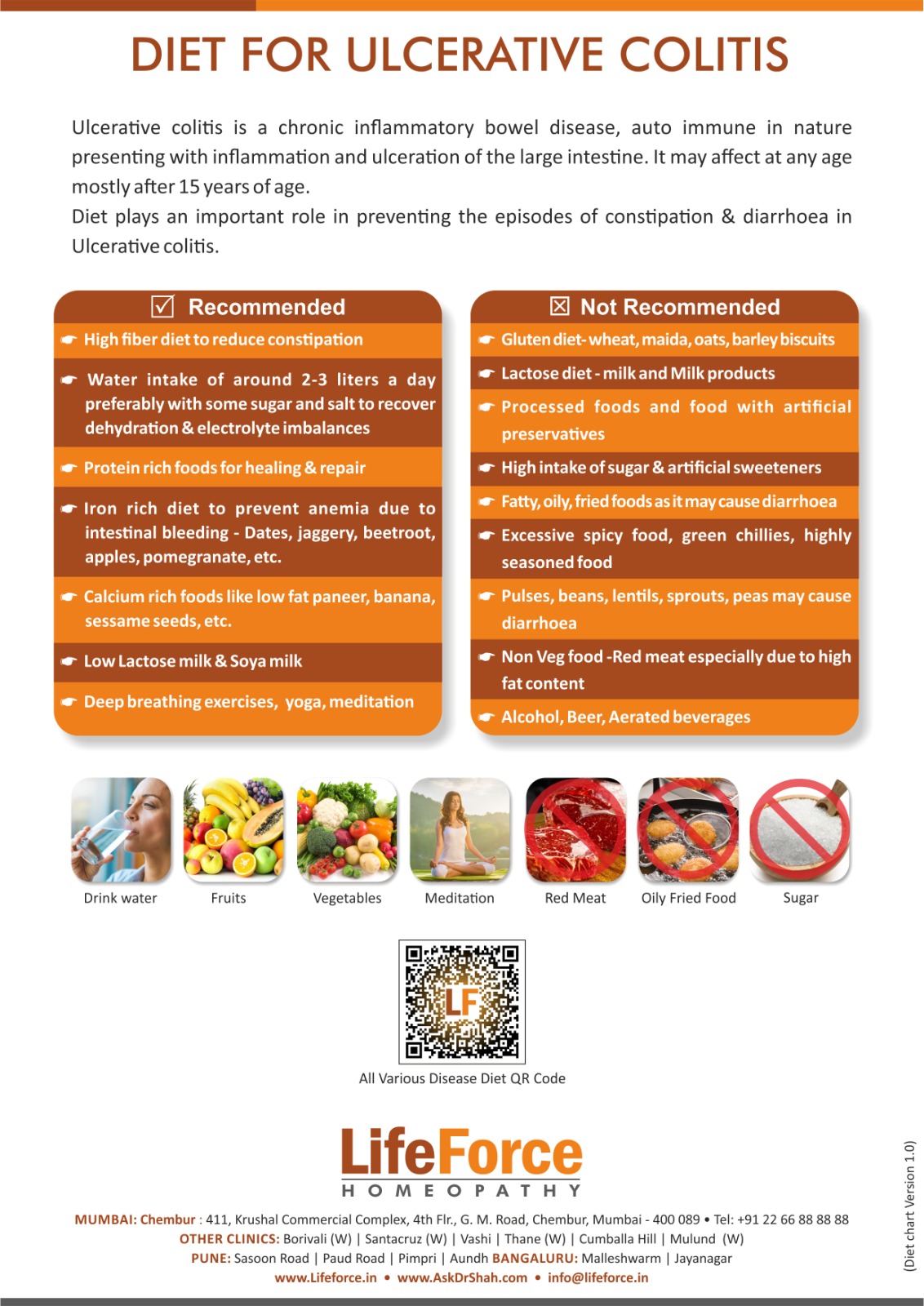
Dietary advice in Ulcerative Colitis (UC) will vary depending on the site of the disease and the activity of the disease.
Certain things to avoid in UC:
- Processed foods (i.e. foods containing preservatives)
- High intake of sugar and artificial sweeteners
- Excess of spicy foods
- High fat and deep-fried foods
- Alcohol, beer, and aerated water
Diet when the patient is relatively symptom-free:
The basic dietary principles for UC are no different from those for the general population. Carbohydrates (rice, bread, pasta, potatoes, breakfast cereals, etc), proteins (pulses, meat, fish, eggs, nuts, etc.), vegetables, and fruits form the main part of the diet. Protein foods are essential for growth and repair and also provide iron - these should be taken in adequate quantities. Fat intake must be moderate because an excess of fat intake may cause wind and diarrhea.
Dairy foods, which provide calcium and protein, should be taken in adequate amounts provided they don't cause any problems (such as diarrhea and wind) to the patient.
Usually, small amounts of milk, for example in tea or coffee, do not cause any problems. Dairy products such as butter, cheese, and yogurt are also well tolerated. If milk is excluded, it should be replaced with low lactose milk or with Soya milk. This should be discussed with a dietician to ensure that the nutritional balance is maintained.
Beer or other alcoholic drinks, excess of fruit or fruit juice, onions and spicy foods aggravate the symptoms in some patients and hence these are better avoided by them.
Constipation is often associated with distal colitis and may aggravate the condition; therefore, it is important to eat sufficient fiber in the diet in order to prevent this. However, if dietary fiber cannot be tolerated without unpleasant symptoms, a bulking agent is advised instead (e.g. Methylcellulose, Fybogel or Normacol), with increased fluid intake to soften and regulate the motions.
Diet during the acute phase of UC:
An inflamed large intestine may not be able to reabsorb sufficient water or salt from the bowel and this can result in passing a large volume of diarrhea or semi-solid stool. Fluids need to be replaced during bouts of diarrhea and vomiting to prevent dehydration. Usually, this can be achieved by drinking more liquid but in severe cases, a solution of salt and glucose in water may be prescribed to improve absorption.
During a relapse, high fiber foods such as wholemeal bread, high fiber breakfast cereals, dried fruit and pulses, beans, lentils, peas, and sprouts, may make diarrhea worse. Reducing fiber may help reduce bowel movements. When symptoms improve, fiber can be gradually reintroduced back into the diet to the level that is tolerated. Those who suffer from constipation or who are troubled by passing hard stools need to maintain an adequate level of fiber in the diet. Bulking agents, stool softeners or osmotic laxatives may be helpful.
When the intestine is inflamed its capacity to absorb fat is impaired and even a moderate amount of fat in the diet may cause wind and diarrhea. Restricting high-fat foods may help. However, it is important to replace these foods with carbohydrate- and protein-rich foods to prevent weight loss.
Protein loss can occur from leakage of the damaged intestinal lining. If this lining bleeds there is a risk of becoming deficient in iron which can lead to anemia. A nutritious diet, high in calories and protein, is then needed to replace lost energy and nutrients.
In active inflammation, certain vitamins and minerals may be lost from the body. Supplements of multivitamins and iron tablets may help. A high intake of fluids and foods rich in magnesium and vitamin C may lower the risk of relapse.
Written & Approved by-
Dr. Rajesh Shah
M.D. (Hom.)