What is Psoriasis?
Psoriasis is a chronic disease on the skin due to a disturbed immune system. In psoriasis, the skin produces an excessive and abnormal amount of skin scales. Normally, skin cells tend to develop deep in one’s skin and rise to the surface gradually. Each skin cell has a lifecycle of about one month. However, in psoriasis-affected individuals, the skin production process takes place rapidly and overproduction of skin cells occurs leading to patchy, scaly skin. Psoriasis is characterized by red, raised, scaly skin patches on the skin’s surface. Usually, whitish-silver scales happen to develop in red, thick skin patches. At times, cracks may develop in the patches which may bleed. However, psoriasis is not contagious and its lesions are not infectious.
Common Areas of The Body That are Affected by Psoriasis:
Most often, scales of psoriasis develop on the joints, such as knees and elbows. About 15% of psoriasis-affected individuals have psoriasis causing inflammation of the joints and leading to symptoms of arthritis. However, psoriasis can affect any area of your body. Patches of psoriasis may occur on your scalp, neck, hands, palms, face, lower back, soles of the feet, or any other body part. A less common type of this skin disorder may also affect your nails, such as toenails and fingernails, the area around the genitals, and soft tissues within your mouth.


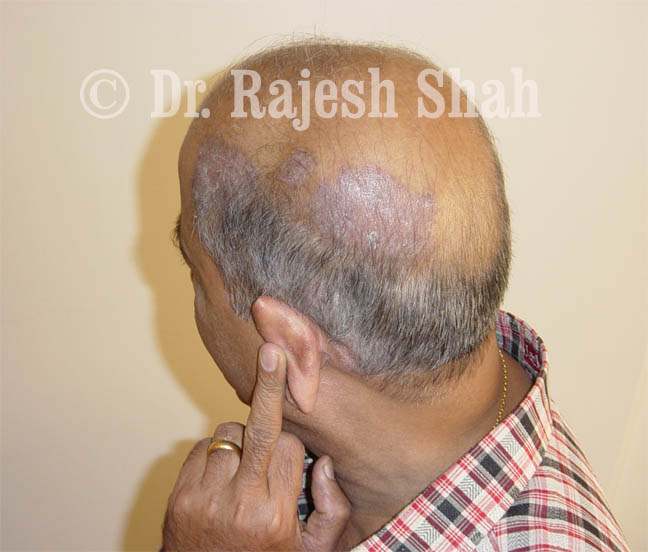

(See pictures where psoriasis affects the back, thighs, legs, area behind the ears, nails, and margins of hair. Most common psoriasis-affected areas are the elbows and knees.)
Ask your questions to Dr. Shah's team directly & get an expert opinion on your ailment!
Grades of Psoriasis:
Based on the percentage of the psoriasis-affected body area and its impact on the quality of life, psoriasis is graded as severe, moderate, or mild. The Psoriasis Area Severity Index (PASI) is an index parameter that helps express how severe the psoriasis is. It comprises three clinical signs, namely erythema (i.e. redness), induration (i.e. thickness), and desquamation (i.e. scaling). The severity of the psoriasis parameter is calculated on a scale of 0 to 4.
The Occurrence of Psoriasis:
Psoriasis tends to appear and disappear with medicines or without medicines. Such phases are called Remissions and Relapses. At times, the patches of psoriasis vanish (which is called remission), while, in some instances, the patches reappear (which is called a relapse). Longer remissions and minimum and shorter relapses give great relief to psoriasis in an affected individual.
Factors Affecting Psoriasis:
Certain factors can trigger a flare-up making the psoriasis patches reappear in a short time span. Factors, such as stress, skin injuries, infections, medications, climate, obesity, tobacco, genetic factors, and alcohol, are some common psoriasis causes that you should watch out for.
On the contrary, certain factors, such as sunlight, tend to alleviate the discomfort and intensity of psoriasis.
How Commonly Psoriasis Occur?
Usually, 1% -2% of the general population is affected by this chronic skin condition. Psoriasis occurs in both males as well as females in equal proportions. An individual can get affected by psoriasis at any age, however, most often, psoriasis occurs in grown-ups between the age groups of 15 and 35 years. Psoriasis can affect children as young as one-year-old babies.
How does Psoriasis Affect our Body?
The skin comprises two layers, such as an inner layer (called the dermis) and an outer layer (called the epidermis). Skin cells that make up the upper layer grow in the inner layer and then move upwards. New cells developed in the dermis replace the old cells of the epidermis at a typical interval of 28 to 30 days.
However, in psoriasis, the cell formation process in the inner layer is accelerated. So, a greater number of new cells are formed in the inner layer and they move upwards to the upper layer at a faster rate than normal. As a result, excess skin cells conglomerates lead to scales and patches of psoriasis.
Also Read: What are the triggers of psoriasis and how to manage it?
Causes of Psoriasis:
Even though the exact cause of psoriasis is not yet clear, it is known to develop due to the body’s internal disharmony and certain environmental triggers. Psoriasis causes include genetic predisposition and disturbed immunity. Certain internal and external factors also cause psoriasis.
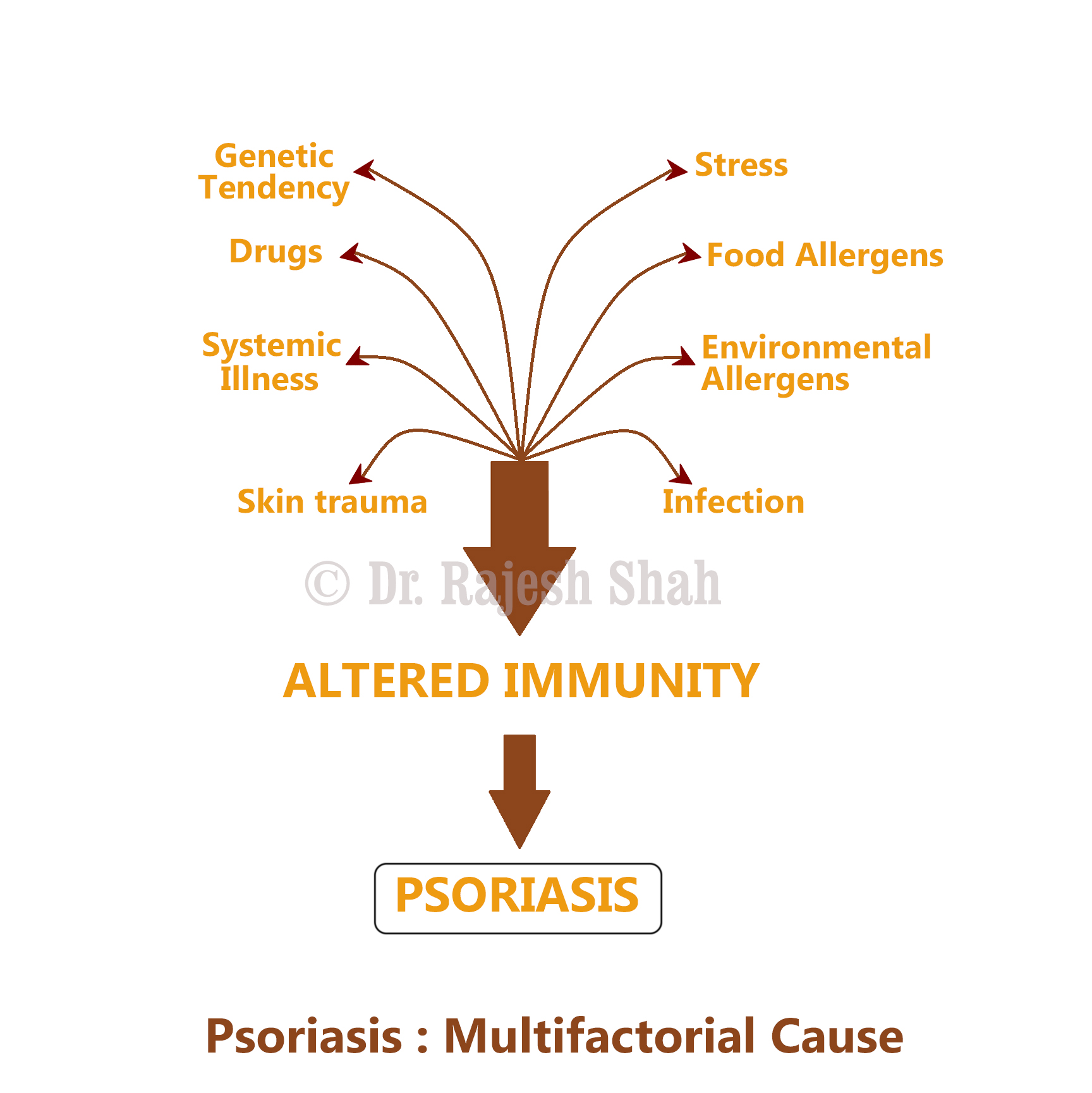
Internal Factors:
- Defective/Disturbed Immune System: The latest medical research reveals that psoriasis results due to a disturbed or defective immune system. An overactive immune system tends to create inflammation in your body. It produces excessive healthy skin cells, and they are pushed to the upper surface of the skin quite quickly resulting in psoriasis.
- Genetics & Heredity: Some of the most prominent psoriasis causes are genetic and hereditary factors. One out of every 3 individuals affected by psoriasis happens to have a relative suffering from psoriasis.
External Factors:
Psoriasis-affected individuals may experience that at certain times their skin condition and discomfort turn worse. Certain factors or conditions that cause relapses or flare-ups of psoriasis are called triggers of psoriasis. Some of them are mentioned below.
- Climate: Often, the onset of the cold climate can trigger a flare-up of psoriasis. On the contrary, hot and sunny weather can provide relief from this skin condition.
- Skin Injury: Physical trauma, such as skin injuries due to an accident, scrape, sunburn, or cut, can cause psoriasis. Psoriatic lesions may occur at the site of skin injury after 10 to 14 days of the injury. Also, vaccines and shots can cause an outbreak of psoriasis.
- Infections: Psoriasis causes also include skin infections and systemic (integral) infections. Upper respiratory infection, HIV infection, and strep throat are some of the common systemic infections that may make you suffer from psoriasis or trigger a flare-up of the same. Besides these, skin infections causing boils and ulcers can also trigger psoriasis lesions.
- Stress: Another common factor that can be the cause, as well as the trigger of psoriasis, is stress. Psychological stress affects both the mind and body of an individual. So, unusually intense stress can trigger a relapse of psoriasis. To prevent the flare-ups of this skin condition, you need to learn to manage and minimize the stress.
- Certain Medications: Lithium or medications which treat depression, beta-blockers that regulate high blood pressure, mepacrine, antimalarials, and NSAID can lead to psoriasis or trigger a relapse of a psoriasis flare-up.

Symptoms of Psoriasis:
Psoriasis usually occurs starting with small, red bumps on the surface of the skin which progress to larger, scaly psoriasis patches. Some of the common symptoms of this skin condition are as follows:
- Red, inflamed and raised skin patches
- Burning and itching affecting the psoriasis lesions
- A white crust of silvery scales surfacing the red patches
- Soreness is present around the lesions
- Dry skin which may crack or even bleed
- Swollen and painful joints
- Thick, pitted nails
Types of Psoriasis:
There are several variants of psoriasis. Some of the common types of psoriasis are as below.
- Plaque psoriasis: The most common type of psoriasis which is observed in the majority of psoriasis patients is plaque psoriasis or psoriasis vulgaris. It results in red, raised, inflamed, and thickened patches of red skin, which are often covered with whitish-silver plaques. You can find these plaques on the knees, elbows, and scalp.
- Scalp Psoriasis: Another common type of psoriasis is scalp psoriasis, which is relatively quite difficult to treat. You may have it only on your scalp or together on your scalp and skin. In several cases of scalp psoriasis, it lasts for many years before it affects the body. Most often, mild psoriasis which affects the scalp is inappropriately identified and treated as dandruff.
- Pustular Psoriasis: This variant of psoriasis is quite common among adults. It is characterized by white blisters which are filled with pus and the broad areas tend to turn red and inflamed. Typically, this type of psoriasis is restricted to the body’s smaller areas, such as feet and hands, however, it may even be widespread.
- Erythrodermic Psoriasis: This type of psoriasis is quite rare but severe. Often, it affects large areas of the body at once. It causes intense redness, swelling, itching, and pain. The skin of the affected person appears to be almost sunburnt. Scales that are formed tend to slough off in big sheets. The patient may also suffer from fever or fall sick. This type of psoriasis can be life-threatening, so those who are affected by it should consult a doctor immediately.
- Guttate Psoriasis: Guttate psoriasis commonly occurs in childhood. It is characterized by small pink spots on the legs, trunk, arms, and scalp. Thick or raised spots like psoriasis patches develop very rarely.
- Palmo-Planter Psoriasis: It is one of the common types of psoriasis which affects either sole, palms, or both. Thickening and scaling of the affected skin area occur along with painful, deep fissures on the affected soles and palms. Certain substances, such as cleaning and washing products and detergents, tend to irritate these psoriasis lesions and obstruct them from healing.
- Inverse Psoriasis: This variant of psoriasis causes red, inflamed, shiny lesions in the folds of skin of the affected body areas. Inverse psoriasis patches develop under the breasts or armpits, around the skin folds present near the genitals, and in the groin. It causes increased sweating and sensitivity to friction, and it can be quite itchy or painful.
- The Psoriatic Nail: About 50 % of psoriasis-affected individuals have psoriasis affecting their toenails or/and fingernails. At times, psoriasis may affect only nails and no other part of the body. The nail may develop yellow to yellow-pink discoloration or the nail plate may get depressed or deeply pitted crumbling into yellowish patches. At times, the affected nail may be lost completely.
- Psoriatic Arthritis: One of the most difficult types of psoriasis is psoriatic arthritis where you suffer from psoriasis along with discomforting joint pain. It can affect any joint of your body. A good psoriasis homeopathic treatment may help psoriasis cure if it’s diagnosed and treated in earlier stages.

How does Psoriasis Affect Social & Mental Health?
At times, psoriasis is so mild that it goes unnoticed. So, it doesn’t affect the individual psychologically or socially. On the contrary, there are psoriasis-affected people who have patches of psoriasis everywhere on their bodies. These individuals may suffer emotional distress, discomfort due to itching and pain, and restricted motion of the affected joints. Besides this, psoriasis patches impart an unpleasant appearance to the person. Chronic itching and flaking bring embarrassment when getting social. Even though it’s not a life-threatening condition, it largely impacts the lifestyle and self-esteem of the affected person adversely. Often, psoriasis is misunderstood and it brings awkwardness and embarrassment while carrying out social interactions. As a result, the psoriasis patient may suffer emotional problems, such as anger, depression, anxiety, and inferior complex.
Diagnosing Psoriasis:
- Physical Examination: Usually, the doctors diagnose psoriasis clinically by examining the affected skin carefully, considering the family history and medical history, and the spread on the affected body parts. A simple physical exam is enough for physicians to diagnose psoriasis.
- Biopsy: When the symptoms are not clear or when the doctor feels the need to confirm the possible or suspected diagnosis, then they may suggest a biopsy. A small sample of the affected person’s skin is taken and sent to a lab for examination under a microscope. It diagnoses not only whether it’s psoriasis or not, but also the type of psoriasis. It helps rule out the possibility of other skin infections or disorders.
Available Treatment Options For Psoriasis:
Psoriasis is indeed a difficult skin condition to treat. In fact, treating psoriasis is quite challenging for the medical science and faculty since, in most cases, after using any modern or available treatments, psoriasis happens to relapse.
Several therapies and methods exist when it comes to psoriasis cure. Most methods offer positive outcomes lasting for varying timespans. Some of the popular treatments available for alleviating psoriasis include allopathic treatment (conventional medicine), psoriasis homeopathic treatment, Ayurvedic treatment, herbal remedies, phototherapy, acupuncture, psoriasis home remedies, and many other treatments. Also, psoriasis treatment can utilize various modes of administration, such as topical application of oils, creams, or lotions, injections, oral medications, the use of UV rays, and the use of needles when treating with acupuncture therapy.
Conventional Treatment:
Conventional medicines, more commonly known as allopathic or modern medicine, use the medicines mentioned below for treating psoriasis. These are immunosuppressive medications in some way or the other.
- Psoralen (with or without P-UV rays) (Oral)
- Retinoids (Oral)
- Methotrexate (Oral)
- Cortisone (Oral, injections, topical)
- Cyclosporine (Oral)
Also Read: Dos and don’ts for the best psoriasis treatment
Psoriasis Homeopathic Treatment:
Psoriasis is not an external or superficial condition but an intrinsic or deep-seated disorder resulting due to a disturbed immune system or genetic or hereditary factors. To treat this disease occurring due to the body’s internal disharmony, well-planned and deeply working medications are necessary. Even though cortisone (by the conventional treatment) may succeed in suppressing the symptoms of the disease, it can’t cure this skin ailment. On the contrary, homeopathy is quite effective in stimulating the natural healing mechanism of the body of the affected individual and restoring the disrupted immune system to normalcy.
Psoriasis homeopathic treatment focuses on treating the immunological factors which tend to cause psoriasis. Various factors, such as physical, genetic, hormonal, environmental factors, and many others, affect your immune system. So, homeopathy aims the recovery by taking into consideration the totality of the individual suffering from psoriasis.
Homeopathic medicines are easy to have as you always need to take them in the form of oral pills through the mouth. Homeopathy does not recommend the application of any medical matter on your affected skin to treat it, except for a good moisturizer. The application of a good moisturizer is a crucial part of the psoriasis treatment, no matter what kind of medication you are having as a primary treatment. It helps you have great relief from excessive dryness and scaling of the skin, itching, and flaking.
Also Read: Homeopathy a boon in psoriasis
How Does Homeopathy Work and Prove Beneficial For Psoriasis Patients?
Psoriasis homeopathic treatment works wonders for psoriasis. Here are some benefits of homeopathy for psoriasis.
- Homeopathy stimulates the body’s innate healing process.
- It addresses the genetic tendencies effectively.
- Homeopathy acts at the root level and effectively restores the disturbed immune system to normalcy.
- It controls the tendency of relapse significantly.
- Homeopathy utilizes ultra-minute amounts of natural medicinal substances providing an effective psoriasis treatment that is completely free from side effects.
- Psoriasis homeopathic treatment offers you long-lasting relief and aids to cure the disease completely over a period of time.
Also Read: Psoriasis treatment
Duration of Course of Homeopathic Treatment for Psoriasis:
Psoriasis is an obstinate condition that is often chronic. And, there is no shortcut to get rid of it. The duration of psoriasis homeopathic treatment varies from patient to patient based on the following factors.
- Duration of psoriasis
- The extent of the spread of the disease. For instance, psoriasis affecting just the skin is easier to treat, however, psoriasis affecting the joints is quite difficult to treat relatively.
- Previous medication (The extensive and long-term use of oral cortisone may prolong the course of psoriasis treatment).
- Affected areas. For instance, psoriasis affected nails and scalp and takes a long duration to treat it.
- Associated ailments and general well-being
Side-Effects of Other Treatments:
- Cortisone: The use of cortisone for treating psoriasis tends to make you dependent on it and cause a rebound effect. Once you use the cortisone for alleviating this skin condition, you are likely to use it again as psoriasis may relapse after you stop using it. You might find it difficult to tackle a psoriasis flare-up by using mild medicines, as, most possibly, you may need to use a higher dose of cortisone to regulate it. Thus, it develops a vicious cycle.
- Topical treatment: As psoriasis is a skin ailment, any common man might think that the application of some medicine on the affected skin can help treat it. However, psoriasis is a disease reflecting on the skin and it’s not an ailment of the skin. This means that psoriasis is an internal condition resulting due to a disturbed immunological system and it affects the skin adversely. So, the topical treatment for the same would be superficial and lasting for a short span of time. After treating a few thousand psoriasis patients at Life Force, we can say that when the topical method is used for psoriasis treatment, the disease happens to relapse invariably.
- Retinoids: Although you may find that retinoids treat the symptoms and discomfort of psoriasis quite effectively, the symptoms are likely to reappear once you curb using them. The side effects of retinoids are a loss of hair, inflammation of the lips, and birth defects in newly born infants if it’s been consumed while expecting.
- Cyclosporine: Kidney problems, poor or weakened immunity, and high blood pressure are some of the adverse effects of cyclosporine.
- Methotrexate: A prolonged use of methotrexate can result in liver damage and a considerable reduction in the red blood cells and white blood cells in your body system.
- PUVA: Some common adverse effects of PUVA for psoriasis are itching, nausea, and burning sensation.

6 Effective & Helpful Tips For Psoriasis:
1. Avoid Scratching:
You might experience an itch and get a feel to scratch your itchy, inflamed psoriasis patch. However, scratching the affected skin area can worsen the condition, cause skin damage, and make you susceptible to a skin infection. So, resist your urge of scratching the skin. Cut your nails timely to maintain clean and short nails. You can also use hand gloves to keep scratching hazards at bay.
2. Manage Stress:
In most cases of chronic psoriasis, psoriasis-affected individuals are prone to low self-esteem, depression, anxiety, and suicidal thoughts. So, it is important to minimize your stress in order to control your mental and physical health. Find and follow different ways, such as meditation and yoga, to beat stress. Join a support group. Go for counseling to relieve your stress.
3. Follow a Healthy Psoriasis Diet:
One of the crucial parts of psoriasis treatment to manage its flare-ups is to follow a healthy psoriasis diet. Make sure your psoriasis diet contains foods abundant in omega-3 fatty acids, such as salmon, mackerel, tuna, and other fishes and foods, kale, fresh fruits, garlic, squash, and fresh vegetables to control the inflammation. Try to avoid having foods containing gluten, such as pasta and bread, since they might trigger a relapse. Ensure you consume plenty of water daily. Besides this, having continuous and sound sleep can help. Also, perform exercises regularly.
4. Go For Warm Baths:
When suffering from psoriasis lesions, avoid having hot water baths as the hot water may cause irritation to your skin. Instead, have warm baths. Add some soothing olive oil and Epsom salt to the lukewarm water and bathe with it. This helps soothe your irritating and itchy skin and provides you with a great relied.
5. Stay Away From Triggers:
One of the effective ways to avoid the relapse of psoriasis is to avoid its trigger. Also, staying away from the possible psoriasis triggers promotes psoriasis cure, as it reduces the possibility of its flare-ups. So, first try to find out your psoriasis triggers, such as stress, certain foods, weather conditions, or medications, and make sure you keep yourself away from them to avoid the risk of psoriasis flare-ups.
6. Quit Smoking & Drinking Alcohol:
Smoking and drinking alcohol can have an adverse effect on psoriasis, as these unhealthy habits can interrupt the periods of remission, trigger psoriasis flare-ups, and reduce the positive effect of psoriasis treatment and psoriasis home remedies. So, it is best to avoid smoking and stay away from alcohol. If you are finding it difficult to avoid these habits, consult a doctor to get help to quit smoking and drinking alcohol.
Also Read: Skincare tips for psoriasis
Are Vitamin Supplements Beneficial In Managing Psoriasis?
Even though psoriasis does not occur due to the deficiency of any vitamin, having certain vitamin supplements can help promote the recovery from psoriasis. If you suffer from excessive flakiness due to psoriasis, having an adequate dose of vitamin D3 and vitamin B12 can prove helpful in obtaining relief from the same.
Psoriasis Diet:
Even though psoriasis is not a dietary ailment, it’s been noticed that the intake of certain unhealthy foods could damage the general health and worsen psoriasis. Avoiding such foods that would trigger or worsen psoriasis could help manage the condition. At Life Force, it’s been observed that eliminating or minimizing the intake of animal proteins in the form of red meat can pace up the recovery from psoriasis. Besides, having a gluten-free diet can prove helpful to several psoriasis patients. Eliminating fatty foods, artificially flavored foods, dairy products, and processed foods too can prove beneficial in minimizing the symptoms and discomfort resulting due to psoriasis. Following a healthy psoriasis-diet play a crucial role in treating this skin condition. Make sure your psoriasis diet comprises omega-3-rich foods, such as pumpkin seeds, flaxseeds, walnuts, and olive oil.
Also Read: 10 Foods that make psoriasis worse
What Could Be The Future of Psoriasis?
Even though psoriasis is not dangerous or life-threatening ailment, it’s known to be a chronic condition that may affect for a long period of several years and its course differs from patient to patient to patient. Also, psoriasis is known for its unique tendency to relapse after a timespan. The intensity of psoriasis ranges from mild to moderate to extremely extensive. And, once just cannot predicate the spread of the disease.
Quite rarely, psoriasis causes long-lasting complications having an adverse impact on vital body organs
Usually, psoriasis is a medico-social ailment, particularly when it surfaces on visible areas of the body, such as over the face. Also, at times, psoriasis affects the patient’s career progress as the employers are unaware of the nature of this disease. Besides this, you may also find psoriasis-affected individuals avoiding leisure activities out of the fear of rejection and embarrassment. Often, this disorder makes the patient feel unattractive and unpleasant to the opposite sex.
So, the future of psoriasis relies on its early detection and timely treatment. If you treat psoriasis by going for immunosuppressive medicines, such as methotrexate or cortisone, then there are chances that it may reappear with greater intensity and you may find it even more difficult to tackle it. As per our experience, choosing psoriasis homeopathic treatment can be highly beneficial. Early detection of this condition and treating it with homeopathy can help you achieve in the future to gain overall control of the ailment effectively and safely without any side effects.

Written & Approved by-
Dr. Rajesh Shah
M.D. (Hom.)